Efficient and effective integration of healthcare with other rehabilitative initiatives is essential to reducing recidivism, according a report from The Pew Charitable Trusts released on Oct. 18.
“Emerging research suggests that underlying health issues, particularly substance use disorders and mental illness, contribute to incarceration and recidivism, and that treatment, combined with seamless care continuity for individuals when they return to communities, can help prevent both,” the report stated.
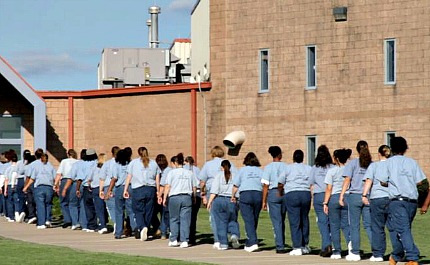 “The stakes for success are high because recidivism comes at great public safety and fiscal cost,” the Pew report said. (Photo: EthicsDaily.com)Prison healthcare services accounted for $18.1 billion nationwide in 2015 – roughly 20 percent of total prison spending. Services are usually administered through a combination of state-employed and contracted providers.
“The stakes for success are high because recidivism comes at great public safety and fiscal cost,” the Pew report said. (Photo: EthicsDaily.com)Prison healthcare services accounted for $18.1 billion nationwide in 2015 – roughly 20 percent of total prison spending. Services are usually administered through a combination of state-employed and contracted providers.
“State prison systems typically provide primary care and basic outpatient services in-house,” Pew Trusts explained. “But nearly every system’s facilities are at least somewhat limited in the care that can be provided … so prison systems must rely to some degree on off-site hospitals for specialist consultations, diagnoses and observation; surgery; and other services.”
The average annual per inmate healthcare expenses are $5,720 with wide-ranging differences between states.
For example, California spent the most in 2015 ($19,796), while Louisiana spent the least ($2,173) despite seeing the highest percent increase in spending since 2010 (56 percent).
A key driver of costs is an aging prison population with one or more chronic conditions (such as cardiovascular disease, asthma and arthritis). While the majority of inmates in all U.S. states were aged 18-39, the 55 and older population has grown substantially in recent years.
“From 1999 to 2015, the number of people age 55 or older in state and federal prisons – a common definition of “older” individuals in prison – increased 264 percent,” the report noted. “During the same period, the number of inmates younger than 55 grew much more slowly: up 5 percent. As a result, older inmates swelled from 3 percent of the total prison population to 11 percent.”
“Twenty-three states reported prioritizing services for individuals diagnosed with a substance use disorder,” the report said. “Twenty-nine states reported that they prioritize re-entry services for individuals with at least one mental health disorder.”
Medication-assisted treatment (MAT) is a common and effective means of helping inmates with drug addiction, yet Pew found that “just 20 states reported facilitating access to MAT upon re-entry.”
Providing quality healthcare services – particularly substance abuse and mental health treatment – to inmates during incarceration and upon release was a focal point of interviewees in EthicsDaily.com’s 2013 documentary, “Through the Door,” which looked at the faith community’s engagement on the prison front.
Linda Leathers, CEO of The Next Door Inc. and a “Through the Door” interviewee, addressed the negative implications of this gap in services and the need to support returning citizens, saying, “When [inmates] are inside, they’re stable on their medication, they’re not using drugs. But what happens when they get on the outside?”
“With nearly all incarcerated individuals eventually returning to society, treatment and discharge planning – especially for those with a substance use disorder, mental illness or infectious disease – play an important role in statewide anti-recidivism and public health efforts,” the Pew report said.
“The stakes for success are high because recidivism comes at great public safety and fiscal cost. By successfully incorporating health care into anti-recidivism strategies, states increase the likelihood that they and their corrections agencies will meet their crime-reduction objectives.”
The full report is available here.
This article originally appeared on EthicsDaily.com.






