(RNS) — The U.S. COVID-19 public health emergency declared under President Donald Trump on Jan. 31, 2020, may be ending on Thursday (May 11), but across the country faith-based groups that provide health care to communities of color say the availability of vaccinations remains important, even if the number of shots they administer is declining.
“I do not believe that we can turn and walk away and say, ‘Hey, OK, we have COVID under control so now let’s just pack up our tools and go home,’” said the Rev. James L. Patterson, CEO of the Partnership of African American Churches in Charleston, West Virginia. “No, we need to continue to deal with the health outcomes that people are suffering.”
The PAAC coordinates with other churches, Catholic Charities, the Salvation Army, and several universities to provide vaccines at 15 clinic locations.
Patterson said his organization has received $7.2 million in funding from federal, state and private sources to help provide vaccines and testing over the last three years. With the slowing of COVID-19 cases, he hopes the partnership, which has already been providing flu shots and glucose and blood pressure checks, will be able to expand to address wider health problems.
“COVID is just the latest pandemic for people of color,” he said. “We’re always in a pandemic. Think about heart disease, diabetes. Those are at pandemic rates in communities of color.”
Over the last few years, African American congregations have provided outsized action on getting people tested and vaccinated.
“Our data shows that not that many congregations served as testing sites and/or vaccination (locations) but almost half of the ones that did were African American,” said Scott Thumma, principal investigator of the Exploring the Pandemic Impact on Congregations project led by the Hartford Institute for Religion Research, adding that “14% of Black churches served as testing or vaccination site compared to 7% of other churches.”
Many African Americans were counting on houses of worship to answer the emergency.
“When FDA made the announcement that the second bivalent was available to 65 plus and immunocompromised, we received phone calls and emails like ‘Are you guys going to have it?’ Fortunately we already had scheduled a clinic,” said the Rev. Carolyn Cavaness, pastor of Bethel African Methodist Episcopal Church in Ardmore, Pennsylvania, which received funding from her county for its work. “They knew that they could come right here to Bethel.”
Cavaness said her church, which also received state support, helped 2,000 people get COVID-19 vaccinations during the pandemic. Dozens of other AME churches outside Philadelphia have been funded by immunization and pediatric organizations to provide vaccines and other health services.
Bethel, which has inoculated about 200 people since January, is not slowing down, though the mix is expected to continue to shift to vaccinations for other maladies. It has scheduled five clinics to continue to provide vaccinations for the flu as well as COVID-19, shingles, and TDAP, which prevents tetanus, diphtheria and pertussis, or whooping cough.
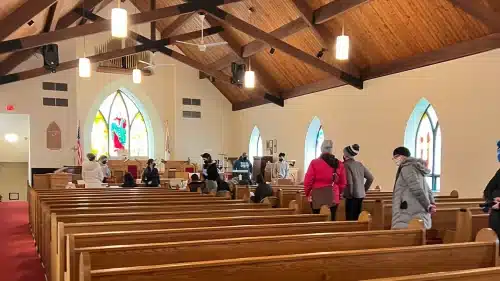
Community members wait in line for vaccinations at Bethel African Methodist Episcopal Church in Ardmore, Pennsylvania, in January 2022. Photo courtesy of Carolyn Cavaness
On Chicago’s South Side, the Inner-City Muslim Action Network’s health center has administered more than 3,400 COVID-19 vaccines and boosters.
“At the height of the pandemic, we were at one time vaccinating approximately 60 patients per day, but that number has decreased over time as more and more people were vaccinated,” said Dabeer Hussain, the organization’s clinical quality manager. “This year, in the past two months, we have given just over 20 vaccines.”
Despite the decrease in demand, Dr. Brittani James, the health center’s medical director, continues to offer the vaccines as she serves those in the community that is predominantly Black and Latinx and about 10% to 15% Arab American.
She recalled the days of the “Delta surge” — when the Delta variant became the most prevalent form of COVID-19 in late 2021 — when “I had somebody swabbing over 200 people single-handedly,” contrasting it with recent days when “numbers have kind of trickled down.”
But James said in a phone interview that she’s aware of continuing need in a community where patients who have experienced health disparities can now receive individualized care.
“It’s all about access,” she said from the retrofitted recreational vehicle that serves as the Inner-City Muslim Action Network’s mobile clinic. “As long as we can do it and there are people who want it, yeah, we’re going to keep going.”
Yusuf Ransome, a scholar at Yale School of Public Health, said his research has shown that some of the areas of New York City that had the highest rates of COVID-19 were areas predominated by African Americans. But his team also found that in the years just prior to the pandemic, many churches in those areas had shut down, depriving not only their members but the surrounding communities of medical support.
Ransome sees potential in the kinds of partnerships between African American churches and health professionals formed during the pandemic.
“I do think that there is room to think about what else can we do beyond the one-per-year kind of diabetes or hypertension screening,” he said. “Can we actually build something much more formal so that we don’t have to wait till the next pandemic to figure out what to do?”
Dr. Miriam Burnett, medical director of the African Methodist Episcopal Church’s health commission, said her denomination is already operating from that perspective. She said her commission is looking ahead, with plans to help schoolchildren have all the other shots they need as they start school in the fall.
“Our plan is to never stop this program,” Burnett said of AME churches like Cavaness’ that continue to provide vaccinations. “The next pandemic is coming around the corner and we want to continue to have in place a mechanism that will allow us to adjust and adjust quickly.”