(RNS) — When it comes to mental health, “too blessed to be stressed” isn’t an altogether helpful catchphrase, according to the American Psychiatric Association.
“You can be blessed and you can be stressed. That’s OK,” said Amy Porfiri, managing director of the American Psychiatric Association Foundation. “We want to hopefully avoid that type of messaging, that it’s a moral failing, that mental health is a spiritual failing.”

Tim Mossholder / Unsplash
For over a decade, the American Psychiatric Association has worked to reduce the stigma around mental health in religious contexts. But while awareness around mental wellness is at an “all-time high,” according to Rawle Andrews, executive director of the APA Foundation, “we still have a lag when it comes to actually accessing care, or giving ourselves permission to access care,” he said.
That “lag” is reflected in a new APA poll released Monday (Sept. 16), which suggests there could be a disconnect between faith communities and the people they serve when it comes to mental health. A survey of over 2,000 participants conducted by Morning Consult on behalf of the APA found that while 60% of U.S. adults say their faith or spirituality is an important factor in supporting their mental wellness, only 52% of those who belong to a religious community agree that their faith community “discusses mental health openly and without stigma.”
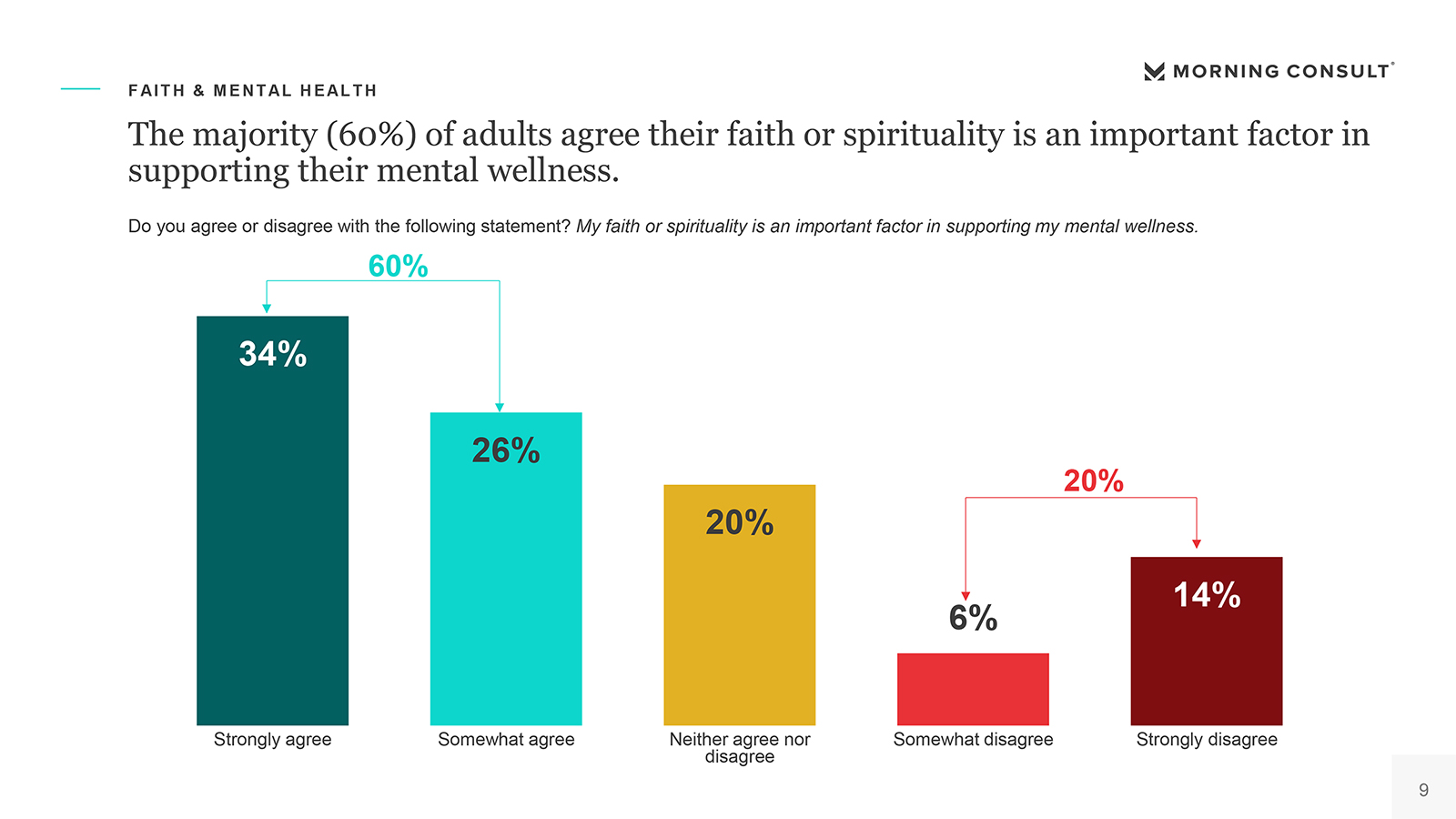
“The majority (60%) of adults agree their faith or spirituality is an important factor in supporting their mental wellness.” (Graphic courtesy American Psychiatric Association/Morning Consult)
When it comes to addressing that gap, findings indicate that faith leaders are key. Of survey participants who belong to a religious community, 57% said they’d be likely to reach out to a faith leader if they were struggling with their mental health, and 68% said they’d be likely to seek mental health care if a religious leader in their community recommended it.
“Our faith leaders have almost become a … first responder when it comes to getting people connected to care,” said Andrews.
Porfiri noted that, anecdotally, parishioners experiencing mental health struggles are often more comfortable turning to a faith leader than making an appointment with a therapist. But faith leaders don’t always receive training on mental health.
“What we learned is that our faith leaders oftentimes very feel ill-equipped,” she said.
Enter the second edition of the APA Foundation’s Mental Health: A Guide for Faith Leaders, released earlier this week. First published in 2015, the guide includes what Porfiri called a “mental health 101” section and recommendations for how and when faith leaders should make a referral to a mental health professional. For instance, the guide teaches faith leaders to consider making referrals for congregants experiencing family dysfunction or prolonged grief or whose emotional and behavioral problems don’t meaningfully improve after six to eight sessions. When making referrals, the guide suggests having a list of qualified professionals on hand and differentiating between clinical care and spiritual support. The guide also lists steps for responding when someone resists clinical treatment.
“I don’t think anything we do with a faith guide is going to make a clinician out of a faith leader, but it certainly will make them turn what we like to say difficult conversations into comfortable or courageous conversations around faith and mental health,” said Andrews.
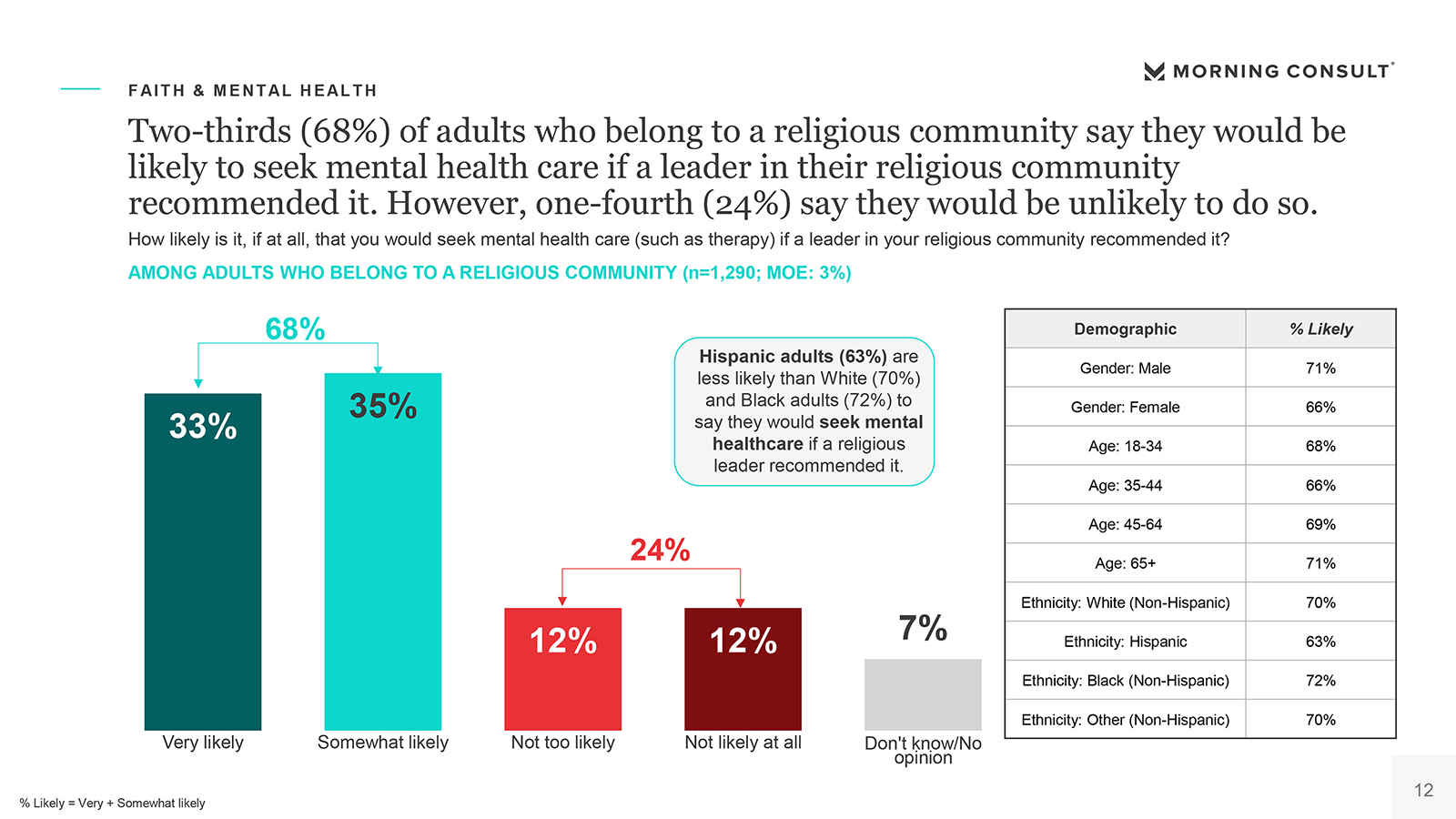
“Two-thirds (68%) of adults who belong to a religious community say they would be likely to seek mental health care if a leader in their religious community recommended it. However, one-fourth (24%) say they would be unlikely to do so.” (Graphic courtesy American Psychiatric Association/Morning Consult)
In light of more recent concerns about clergy burnout, the updated guide makes clear that faith leaders aren’t solely responsible for congregants’ mental health. A new section includes different models for how faith communities can link congregants with clinical services, from embedded or affiliated mental health clinics to simply having a current set of mental health resources on hand. The guide also includes suggestions for dealing with clergy compassion fatigue and burnout, including keeping tabs on symptoms, from emotional numbness to increased irritability and chronic fatigue, and taking steps to delegate tasks, schedule sabbaticals, and build supportive relationships with people outside of work.
“We have to start seeing our faith leaders as human beings as well,” said Andrews. “They can’t just be 24/7, 365. That has to be part of the message.”